Optimising your medical portfolio for Dermatology
Dermatology is a unique specialty with remarkable breadth. It encompasses over 2,000 skin conditions, skin cancer and dermatological surgery, and the care of both children and adults. The specialty also offers extensive opportunities in research, medical education, subspecialisation and private practice. It is therefore no surprise that dermatology is an increasingly competitive specialty.
In the 2025 UK national recruitment round, the competition ratio for Dermatology ST3 was 4.58, with 261 applicants competing for 57 posts. Many applicants require more than one attempt to secure a National Training Number (NTN).

In this article
A rough guide for aspiring dermatologists
This guide aims to provide practical tips on how to maximise your portfolio score, which in turn improves your chances of being shortlisted for interview and ultimately securing a training post.
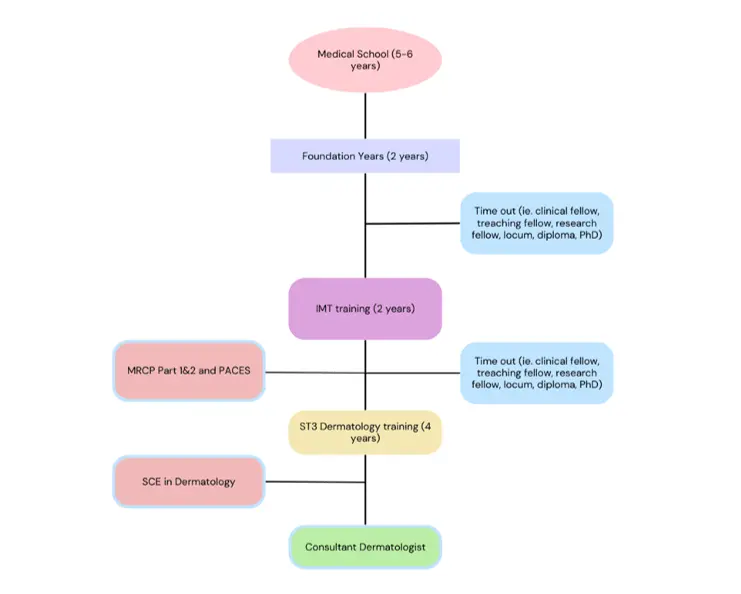
Key:
IMT: Internal Medical Training
NTN: National Training Number
MRCP: Membership of the Royal Colleges of Physicians
ST3: Specialty Training Year 3
SCE: Specialty Certificate Exams
PhD: Doctorate of Philosophy
PACES: Practical Assessment of Clinical Examination Skills
The most common pathway from medical school to becoming a dermatology consultant is illustrated in the flowchart above. Along the way, trainees must complete membership and specialty examinations (MRCP and SCE), and MRCP exams can be attempted as early as foundation year 2 (FY2).
There are also natural pauses in medical career progression that can be used strategically to build clinical, teaching or research experience in dermatology. In addition to the standard training route, an alternative pathway exists: CESR (Certificate of Eligibility for Specialist Registration). Further details can be found in the ‘Useful links’ section.
Routes into Dermatology training
Following medical school and foundation training, the most common route into dermatology is via Internal Medical Training (IMT). Alternative routes include Paediatrics and Core Surgical Training, although these have additional requirements.
Regardless of entry route, membership of the relevant Royal College (RCP, RCS or RCPCH) is mandatory.
If you pursue the IMT route, you must pass all three parts of the MRCP (Part 1, Part 2 and PACES) before starting an ST3 dermatology post. Dermatology is currently a Group 2 specialty, meaning that only IMT Stage 1 (the first two years of IMT) is required, rather than completion of all three years.
Portfolio-based shortlisting in dermatology
Shortlisting for both IMT and ST3 Dermatology is based on portfolio self-assessment scores across defined domains.
- IMT: 7 domains (new introduction of ‘Unique Applicants to IMT’ for 2026 recruitment round)
- ST3 Dermatology: 7 domains (MRCP included as opposed to points for Unique Applicants)
Importantly, many scoring domains do not need to be dermatology-specific, so relevant opportunities in any specialty should be used to your advantage.
Commitment to the dermatology specialty
For ST3 Dermatology, the ‘Commitment to Specialty’ domain is scored out of 20 points by two interviewers. At the time of writing (January 2026), this domain does not contribute to shortlisting and is assessed at interview.
Application Scoring:
Postgraduate degree (max 4 points)
Typical scoring includes:
- 1 point – Diploma or Postgraduate Certificate (PGCert), usually lasting 1–12 months
- 4 points – PhD (typically 3 years)
Ways to achieve this include:
- Applying for a Specialised Foundation Programme (SFP) with a teaching or leadership focus, some of which offer a PGCert
- Taking time out of training or undertaking a teaching fellow role (often linked to PGCert qualifications)
- Completing a diploma, including dermatology-specific options
The Primary Care Dermatology Society (PCDS) provides guidance on dermatology diplomas.
Overall, this domain requires a significant investment of time and money for relatively few points. Many applicants may benefit from prioritising other sections first.
Presentations (max 6 points)
- Local oral presentations (e.g. presenting a project within your GP practice or hospital department) score points
- National or international oral presentations score maximum points
- Poster presentations also score and are often easiest to obtain
Practical tips:
- Submit abstracts from audits, QIPs or research projects
- If oral presentation slots are unavailable, apply for poster presentations
- The RCP and other organisations offer accessible poster competitions
- Search widely for conferences and submit abstracts — persistence pays off
This is a highly achievable domain and well worth prioritising.
Publications (max 8 points)
This domain is often opportunity-dependent.
- Seek out supervisors willing to involve you in projects
- While on placement, express interest to senior clinicians — many have case reports or projects needing support
- SFP posts and intercalated degrees are good opportunities to publish
- Well-designed QI projects can be published if methodology and implementation are robust
The Future Healthcare Journal actively encourages trainee-led, high-quality QI submissions.
Teaching (max 5+3points)
This domain has two components:
1. Organising and delivering teaching (up to 5 points)
Points depend on:
- Target audience (local, regional or national)
- Your level of involvement
Key requirements:
- A regular programme delivered over at least 3 months
- Evidence of a timetable, feedback and a consultant supervisor letter
Tips:
- Identify a gap in local teaching
- Collaborate with colleagues and deliver teaching less frequently (e.g. fortnightly) to maintain sustainability
2. Teaching qualifications (up to 3 points)
Options include:
- Free online courses (e.g. Open University)
- Face-to-face or online courses funded via your study budget
- Local courses recommended by postgraduate medical education departments
- RCP ‘Teach the Teacher’ courses
Quality Improvement (max 4 points)
- GP placements are excellent environments for QIPs
- Most departments support audit and QI work
- Aim to lead the project and complete multiple PDSA cycles to maximise points
QIP involvement is a mandatory requirement for both Foundation and IMT training, making this a high-yield and essential domain.
*Strong QIPs can often be developed into presentations or publications*
Additional Sections for Higher Specialty Training:
Commitment to Dermatology (interview only)
- This section must be dermatology-specific. Useful strategies include:
- Joining (or establishing) a university Dermatology Society
- Completing dermatology rotations during Foundation or IMT
- Attending clinics on study days
- Undertaking taster weeks or electives
- Engaging with dermatology charities
- Building relationships within your local dermatology department and identifying a mentor
- Becoming a member of the British Association of Dermatologists (BAD)
- Attending dermatology conferences
- Writing reflections or case reports
- Volunteering with educational resources such as DermNet NZ
MRCP
- MRCP Part 1, Part 2 and PACES are mandatory before starting an ST3 Dermatology post
- MRCP carries significant weight in applications and should be prioritised early
- You can start sitting MRCP exams from Foundation Year 2
Useful links
Competition ratios
IMT self-scoring
Higher Specialty Scoring
BAD events
RSM prizes
CESR pathway
FHJ Submissions
RCP events/conferences
RCP teach the teacher course
Bristol QI Conference
I hope you have found these tips useful. If you have any questions don’t hesitate to contact me on LinkedIn or email me on jemima.sellicks@nhs.net.
Please note the information on this post are factually correct as of January 2026. Self-application scores and competition ratios are subject to change.
Dr Jemima Sellicks IMT Doctor with interest in Dermatology
RCP East Midlands Representative
Future Healthcare Journal, Assistant Editor
Dr Gavin Fong Specialist Registrar in Dermatology
University Hospitals of Derby and Burton
Donate to us now
By donating to skin disease research, you are helping us to find treatments and cures for common conditions like rosacea, acne and psoriasis through to potential killers like melanoma skin cancer. Thank you.